Decoding ANA Positive ICD-10: Understanding the Diagnosis and Implications
Navigating the complexities of medical diagnoses can be daunting, especially when encountering terms like “ANA positive.” This article aims to demystify what an ANA positive result means in the context of ICD-10 coding, providing a clear understanding of the associated diagnoses and their implications. The term “ANA positive” refers to a positive result on an antinuclear antibody (ANA) test, a common blood test used to help diagnose autoimmune disorders. When this result is translated into medical coding, specifically using the International Classification of Diseases, Tenth Revision (ICD-10), it becomes crucial to understand which codes are applicable and why.
What is ANA and Why is it Tested?
Antinuclear antibodies are antibodies that target the nuclei of cells in the body. Everyone has antibodies that help fight infection and disease. However, in autoimmune diseases, the immune system mistakenly attacks the body’s own tissues, producing autoantibodies like ANA. An ANA test detects these autoantibodies in the blood. A positive ANA test indicates that the immune system may be attacking the body’s own tissues, but it doesn’t definitively diagnose any specific disease. Many healthy individuals can also test ANA positive, albeit often at lower titers. The clinical significance of an ANA positive result is therefore dependent on other clinical findings, symptoms, and additional diagnostic tests.
ICD-10 Coding for ANA Positive Results
The ICD-10 (International Classification of Diseases, Tenth Revision) is a globally recognized system for coding diseases, signs, symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases. It is used by healthcare providers and insurance companies to standardize the reporting of medical conditions. When an ANA positive result is encountered, it’s essential to understand how to properly code it within the ICD-10 framework.
While “ANA positive” itself doesn’t have a direct ICD-10 code, it’s the underlying condition or suspected autoimmune disease that will be coded. Here are some common ICD-10 codes that might be considered in the context of an ANA positive result, depending on the clinical presentation and associated symptoms:
- M32.9: Systemic lupus erythematosus, unspecified – This code is used when the patient’s symptoms and test results, including an ANA positive result, suggest lupus, but a more specific subtype cannot be determined.
- M35.0: Sicca syndrome [Sjögren’s syndrome] – Sjögren’s syndrome is an autoimmune disorder that often presents with an ANA positive result, along with symptoms like dry eyes and dry mouth.
- M05.9: Rheumatoid arthritis, unspecified – Rheumatoid arthritis (RA) is another autoimmune condition frequently associated with positive ANA tests. However, the presence of rheumatoid factor (RF) and anti-CCP antibodies are more specific for RA.
- M33.2: Polymyositis – This is an inflammatory myopathy that can be associated with a positive ANA result.
- M34.0: Systemic sclerosis – Also known as scleroderma, this condition involves hardening and tightening of the skin and connective tissues, often linked to a positive ANA.
- R77.9: Abnormality of plasma protein – This is a more general code that can be used when a positive ANA is found but the underlying cause is not yet determined. It’s often used as a temporary code while further investigations are conducted.
The Importance of Accurate Coding
Accurate ICD-10 coding is vital for several reasons:
- Proper Diagnosis and Treatment: Correct coding ensures that the patient receives the appropriate diagnostic workup and treatment plan based on their underlying condition.
- Insurance Reimbursement: Insurance companies rely on ICD-10 codes to process claims. Incorrect or incomplete coding can lead to claim denials or delays.
- Statistical Tracking: ICD-10 codes are used for statistical tracking of diseases and health trends, which helps in public health planning and research.
- Medical Record Keeping: Accurate coding provides a standardized way to document a patient’s medical history, facilitating communication among healthcare providers.
Clinical Significance and Further Investigation
An ANA positive result is not a diagnosis in itself. It’s a piece of the puzzle that needs to be interpreted in the context of a patient’s symptoms, medical history, and other test results. Here’s what typically happens after an ANA positive result is obtained:
- Review of Symptoms and Medical History: The healthcare provider will thoroughly review the patient’s symptoms and medical history to identify any potential autoimmune disorders.
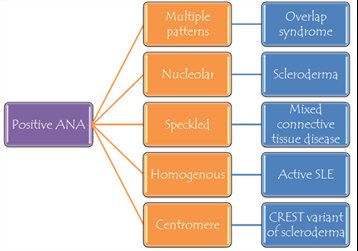
- Titer and Pattern Analysis: The ANA test reports a titer, which indicates the amount of antibodies present in the blood. Higher titers are more likely to be clinically significant. The pattern of the ANA (e.g., homogeneous, speckled, nucleolar) can also provide clues about the possible underlying condition.
- Additional Blood Tests: Depending on the clinical suspicion, additional blood tests may be ordered to look for specific autoantibodies associated with different autoimmune diseases. These tests might include anti-dsDNA, anti-Sm, anti-RNP, anti-SSA/Ro, anti-SSB/La, anti-Scl-70, anti-Jo-1, and others.
- Physical Examination: A thorough physical examination is crucial to identify any signs or symptoms of autoimmune disease, such as joint pain, skin rashes, or organ involvement.
- Imaging Studies: In some cases, imaging studies like X-rays, CT scans, or MRIs may be necessary to evaluate organ involvement.
Common Autoimmune Diseases Associated with ANA Positive Results
Several autoimmune diseases are commonly associated with an ANA positive result. Understanding these conditions can help healthcare professionals and patients navigate the diagnostic process more effectively. Here are a few examples:
- Systemic Lupus Erythematosus (SLE): Lupus is a chronic autoimmune disease that can affect many different organs in the body, including the skin, joints, kidneys, and brain. An ANA positive result is a hallmark of lupus, although not all individuals with a positive ANA have lupus. Other specific antibodies, such as anti-dsDNA and anti-Sm, are also often present in lupus patients. [See also: Understanding Lupus Symptoms and Treatments]
- Sjögren’s Syndrome: Sjögren’s syndrome primarily affects the moisture-producing glands, leading to dry eyes and dry mouth. While an ANA positive result is common, specific antibodies like anti-SSA/Ro and anti-SSB/La are more specific for this condition.
- Rheumatoid Arthritis (RA): RA is a chronic inflammatory disorder that primarily affects the joints. While rheumatoid factor (RF) and anti-CCP antibodies are more specific for RA, a positive ANA can sometimes be present, particularly in individuals with early or severe disease.
- Systemic Sclerosis (Scleroderma): Scleroderma is a rare autoimmune disease that affects the skin and internal organs, causing thickening and scarring. Different subtypes of scleroderma are associated with different ANA patterns and specific antibodies, such as anti-Scl-70 and anti-centromere antibodies.
- Mixed Connective Tissue Disease (MCTD): MCTD is a condition that has features of several different autoimmune diseases, including lupus, scleroderma, and polymyositis. It is often associated with a high-titer ANA and the presence of anti-RNP antibodies.
Factors Influencing ANA Results
It’s important to recognize that several factors can influence ANA results, leading to false positives or false negatives. These factors include:
- Age: The prevalence of positive ANA results increases with age, even in healthy individuals.
- Medications: Certain medications can induce a positive ANA result.
- Infections: Some infections can temporarily trigger the production of ANAs.
- Cancer: Rarely, certain cancers can be associated with a positive ANA.
- Family History: Individuals with a family history of autoimmune disease may be more likely to have a positive ANA, even if they don’t have any symptoms.
Conclusion
An ANA positive result in the context of ICD-10 coding requires careful consideration and clinical correlation. While the result itself does not equate to a specific diagnosis, it serves as an important clue that prompts further investigation into possible autoimmune disorders. Accurate coding, combined with a thorough clinical evaluation, is essential for ensuring that patients receive the appropriate diagnosis, treatment, and care. Understanding the nuances of ANA testing and its implications is critical for healthcare professionals navigating the complexities of autoimmune disease management. The presence of an ANA positive result should always be interpreted in the context of the patient’s overall clinical picture, including their symptoms, medical history, and other laboratory findings. A high titer ANA positive result may warrant more aggressive investigation, while a low titer result in the absence of symptoms may be less concerning. Ultimately, the goal is to provide the best possible care for patients by accurately diagnosing and managing their underlying conditions. Remember that an ANA positive result is just one piece of the puzzle, and a comprehensive approach is necessary for effective patient care. Further research and consultation with specialists in rheumatology or immunology may be necessary to accurately diagnose and manage complex cases involving ANA positive results. In conclusion, understanding the nuances of an ANA positive result and its corresponding ICD-10 codes empowers both healthcare providers and patients to navigate the diagnostic process with greater clarity and confidence. It’s important to always consult with qualified medical professionals for accurate diagnoses and treatment plans related to any medical condition or test result, including an ANA positive test.
